Did you know that about 70-80% of the immune system resides in the gut? This just shows how interconnected our gut health is with our immunity.
From the microbes that live in our gut to the foods we choose to consume, all play a vital role in shaping our immune response and protecting us from illness.
In this article, we’ll break down the science behind the connection between the gut and immune system, highlight actionable strategies to support it, and offer client-facing tips that you can start using on your practice.
The Gut-Immune Connection Explained
The gut and immune system share a symbiotic relationship that begins at birth and evolves across the lifespan. During infancy, microbial colonization of mucosal tissues-particularly in the gut-plays a foundational role in “educating” the immune system, shaping its ability to distinguish harmful pathogens from benign substances.
This early-life dialogue between microbes and immune cells establishes a biological framework that influences health outcomes well into adulthood.
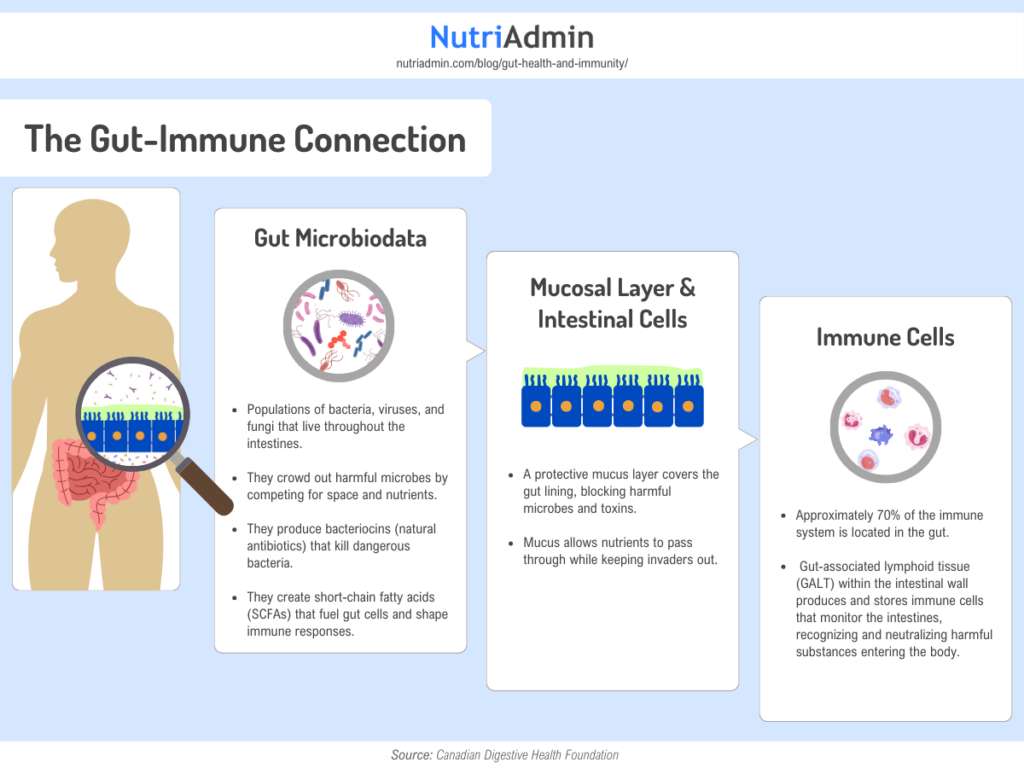
Gut Microbiota
Trillions of bacteria, viruses, and fungi in the gut form a complex ecosystem. In addition, these microbes break down food, produce vitamins, and generate compounds like short-chain fatty acids (SCFAs) that regulate immune responses. Beneficial bacteria, help maintain balance by crowding out harmful pathogens.
Mucosal Layer & Intestinal Cells
The gut lining is protected by a mucus layer that physically separates microbes from the intestinal wall. Specialized cells called enterocytes form tight junctions to prevent unwanted substances from leaking into the bloodstream. Goblet cells secrete mucus, while Paneth cells release antimicrobial peptides to control microbial growth
Immune Cells in the Gut
Over 70% of the body’s immune cells reside in the gut. Key players include:
- IgA-producing plasma cells: Release antibodies that neutralize pathogens.
- Dendritic cells: Regulate responses to food antigens and gut microbes, while also responding to intestinal pathogens. Their role is to help maintain a balance between tolerance and immune activation, contributing to regulatory T cell responses and controlling inflammation in the gut.
- Macrophages: Engulf invaders and produce antimicrobial chemicals
Gut Dysbiosis and Immune Dysfunction
When the balance of gut microbiome is disrupted—known as gut dysbiosis—the immune system can become compromised.
When harmful bacteria outnumber beneficial ones (dysbiosis), they weaken the gut’s protective mucus layer and damage intestinal cells. This creates “leaky gut,” where toxins and undigested food particles escape into the bloodstream. The immune system reacts by flooding the body with inflammatory chemicals like cytokines, which are linked to chronic inflammation, allergies, or autoimmune conditions.
Dysbiosis also reduces production of short-chain fatty acids (SCFAs), compounds made by the “good bacteria” in the gut. SCFAs have significant anti-inflammatory functions and help prevent excessive immune responses. A lack of SCFAs due to dysbiosis can contribute to persistent inflammation and immune dysregulation.
Significant Outcomes
- Nutrient deficiencies: Impaired gut lining reduces absorption of immune-critical nutrients like zinc, vitamin D, and selenium.
- Autoimmune triggers: Chronic inflammation from leaky gut can “confuse” immune cells, making them attack healthy organs.
Nutrients and Foods That Support Gut Health and Immunity
Nutrition is one of the most effective tools for supporting the gut-immune connection, but no single food or nutrient can “boost” the immune system on its own. Instead, a varied diet rich in specific nutrients and food groups helps maintain a healthy gut microbiome and supports immune function.
| Immune & Gut Health Role | Food Sources | |
|---|---|---|
| Fiber | Feeds beneficial gut bacteria, producing SCFAs that strengthen gut barrier, reduce inflammation, and support immune cell function. | Fruits, vegetables, legumes, whole grains, nuts, seeds |
| Prebiotics | Non-digestible fibers that selectively promote growth of beneficial gut bacteria, enhancing immune response. | Garlic, onions, leeks, asparagus, bananas, chicory root, Jerusalem artichoke |
| Probiotics | Live beneficial bacteria that restore microbial balance, improve gut barrier, and modulate immune responses. | Yogurt, kefir, sauerkraut, kimchi, miso, kombucha |
| Vitamin C | Supports immune cell function, antioxidant, promotes skin and gut barrier integrity. | Citrus fruits, bell peppers, strawberries, kiwi, broccoli, tomatoes |
| Vitamin D | Regulates immune responses, supports gut barrier function, and reduces inflammation. | Fatty fish (salmon, mackerel), fortified dairy, egg yolks, mushrooms (sun-exposed) |
| Vitamin A | Maintains mucosal linings (gut, respiratory), supports immune cell development. | Sweet potatoes, carrots, spinach, kale, liver, eggs |
| Vitamin E | Antioxidant, supports immune cell function and gut barrier. | Almonds, sunflower seeds, spinach, avocado, olive oil |
| Zinc | Supports immune cell development, wound healing, and gut barrier integrity. | Oysters, beef, pumpkin seeds, lentils, chickpeas |
| Selenium | Antioxidant, supports immune cell activity and gut health. | Brazil nuts, seafood, poultry, eggs, sunflower seeds |
| Glutamine | Primary fuel for intestinal cells, supports gut barrier repair and immune function. | Beef, chicken, fish, eggs, dairy, cabbage, beans |
Lifestyle Factors That Influence Gut Health and Immunity
Diet is just one piece of the puzzle. Several lifestyle factors also affect the gut and immune system:
- Chronic stress can alter the gut microbiome and suppress immune function.
- Poor sleep can disrupt microbial balance and weakens immunity.
- Overuse of antibiotics can reduce microbial diversity.
- Exercise at moderate levels appears to promote microbial diversity and support immune health
Applying the Science in Practice
Understanding the connection between gut health and immunity is one thing—helping clients apply it in a way that supports long-term health is another. For professionals in nutrition and fitness, this is where evidence meets everyday coaching.
Here are practical ways to assess, educate, and support your clients using the latest science.
Include Gut and Immune Health in Client Assessments
Include questions about digestive symptoms and immune health in your nutritional assessment forms or during assessments in general to identify possible gut imbalances.
- Do you regularly experience symptoms such as bloating, gas, constipation, or diarrhea? If yes, please describe their frequency and severity. (Helps identify common gut health issues and patterns.)
- How many servings of fruits and vegetables do you typically consume each day? Please list examples of your most common choices. (Assesses intake of fiber and nutrients that support gut and immune health.)
- Have you been diagnosed with any gastrointestinal conditions (e.g., IBS, SIBO, celiac disease), allergies, or autoimmune disorders? If yes, please specify. (Identifies pre-existing conditions that may impact gut and immune function.)
- Do you consume fermented foods or probiotics regularly (e.g., yogurt, kefir, sauerkraut, kimchi)? If so, how often? (Evaluates intake of foods that support beneficial gut bacteria.)
- Are you currently taking any medications (including antibiotics or supplements) that might affect your digestion or immune system? (Highlights potential factors that could disrupt gut microbiota or immune balance.)
These questions can help identify patterns that may indicate underlying gut-immune system issues. Reviewing dietary habits, such as fiber intake, consumption of fermented foods, alcohol, and sugar, can provide insights into gut bacteria diversity.
Focus on a Food-First Approach to Support the Gut-Immune Axis
Encourage clients to prioritize whole foods that support gut bacteria and the immune system.
- Plant-based Diversity: Recommend 30 different plant foods per week to encourage microbial diversity, a key marker of gut health.
- High-fiber Foods: Beans, lentils, oats, leafy greens, and seeds are rich in prebiotics that fuel short-chain fatty acid production.
- Fermented Foods: Yogurt, kefir, kimchi, sauerkraut, miso, and tempeh introduce beneficial bacteria to the gut.
- Anti-Inflammatory Fats: Fatty fish, walnuts, flaxseeds, and olive oil help lower systemic inflammation.
- Minimize Ultra-Processed Foods: Diets high in refined sugars and low in fiber have been associated with reduced microbial diversity and increased gut permeability.
Nutrient-Rich Recipes Supporting Gut Health and Immunity
NutriAdmin offers a recipe database filled with gut and immune-friendly options. These recipes include a diverse mix of fruits, vegetables, proteins, and sources of prebiotics and probiotics. You can easily search for a dish you like and add it to a client’s meal plan
In addition to this recipe search feature, NutriAdmin has a meal plan generator that allows you to create personalized meal plans in just 60 seconds.
Feel free to share these delicious recipes from NutriAdmin with your clients:
Support Lifestyle Habits That Influence Gut Health and Immune Function
Beyond food, lifestyle has a significant impact on both gut health and the immune system.
- Sleep Hygiene: Inadequate or irregular sleep negatively alters the gut microbiota and weakens immune regulation. Encourage 7–9 hours per night with consistent sleep-wake cycles.
- Stress Management: Chronic stress can increase intestinal permeability and shift the gut microbiota toward a more inflammatory profile. Techniques such as meditation, breathing exercises, or journaling can be helpful.
- Physical Activity: Moderate-intensity exercise has been shown to enhance gut microbial diversity and reduce systemic inflammation.
Summary
Gut health significantly impacts the immune system, as most immune cells are located in the gut lining. The gut microbiota helps maintain immune balance and protect against pathogens, supported by the mucosal layer and intestinal cells. When gut bacteria become imbalanced, immune dysfunction and inflammation can occur, contributing to various health issues.
Nutritional strategies emphasizing fiber, fermented foods, and plant diversity help maintain a healthy gut microbiome and immune system. Additionally, lifestyle factors such as stress management, exercise, and sleep quality impact this relationship.
Nutrition and fitness professionals can integrate these insights into practice to support clients’ gut and immune health through personalized nutrition and lifestyle interventions.