Have you heard about the AIP disease diet? Who is it for? When can you recommend it? What are the benefits? Is it effective in treating autoimmune diseases? What causes autoimmune diseases? Is there a cure for autoimmune diseases?
As a nutritionist, dietician, or coach, you must have had clients ask some or all of these questions. 1 in 10 individuals suffer from autoimmune diseases globally, making it the third largest prevalent disease category, behind cancer and heart disease. In the US, autoimmune disorders are the second most popular cause of chronic illness.
Even though these conditions affect millions all over the world, their exact causes still remain unclear to date. However, several studies point to an interplay between genetic and environmental factors. Environmental factors such as infections, diet, drugs, stress, and pollutants have all been implicated in the development of autoimmune conditions.
Narrowing on diet, it is impossible to deny the correlation between nutrition and immunity. This is because the immune system comprises some of the most energy-consuming cells in humans.
It is logical that if nutrition provides the fuel for immune cells to function, nutrition is one major factor to examine when there is a malfunction in these cells. Unsurprisingly, research has demonstrated the impact of specific diet patterns on markers of immune function.
While it is true that scientists need to conduct more research to understand the extent of the impact of nutrition on autoimmune diseases, some connections between diet and some autoimmune conditions are already very clear, e.g. Celiac disease and gluten consumption.
Read on to learn more about the AIP disease diet to help your clients and also make you more effective in your practice! Moreover, you can also download sample AIP meal plans for free if you read till the end!
- What are Autoimmune Diseases?
- Risk factors for Autoimmune Disease
- Common Autoimmune Disease Symptoms
- How is Autoimmune Disease Diagnosed?
- What is the Autoimmune Disease Diet?
- How Does the AIP Meal Plan Work?
- When to Recommend the Autoimmune Disease Diet
- How to Make an AIP Meal Plan
- Benefits of the Autoimmune Disease Diet
- Does the Autoimmune Disease Diet have any Risks?
- Self-care Tips for managing Autoimmune Diseases
- Conclusion
- FAQs
What are Autoimmune Diseases?
An autoimmune disease is a “condition in which the body’s immune system mistakes its own healthy tissues as foreign and attacks them.”
In simple terms, in autoimmune diseases, the cells that are supposed to defend the body against foreign, harmful organisms begin to attack the body’s cells and tissues. Consequently, several manifestations or symptoms develop.
Most of the time, autoimmune diseases manifest as inflammation that affects different parts of the body. Depending on the type of autoimmune disease, it may affect a specific organ or tissue or may affect several parts of the body.
There are more than 80 known autoimmune diseases. Examples of autoimmune disorders are Type 1 Diabetes, Rheumatoid arthritis, Multiple sclerosis, Vitiligo, myasthenia gravis, Sjogren syndrome, Systemic Lupus Erythematosus (SLE), and Psoriasis.
Risk factors for Autoimmune Disease
Risk factors increase the chances of developing a condition or disease. For autoimmune disorders, researchers have been able to identify certain risk factors:
Gender
78% of those affected by autoimmune diseases are women. The reasons are not clear, but researchers believe it has something to do with the hormonal profile in women. However, researchers will need further studies to demystify the relationship between gender and autoimmune disorders.
Genetics
While there is no single autoimmune gene, studies have discovered there are gene mutations that can make individuals more vulnerable to immune attacks. The impact of these genes individually is infinitesimal, but when there is an aggregation of their effects, then there is an increased susceptibility to autoimmune conditions.
Obesity
Obesity is a risk factor for several diseases, including autoimmune diseases. More than 10 autoimmune disorders have some connection with excess weight. Obesity plays a role in triggering and prolonging autoimmune disorders. It can lead to a breakdown of the body’s self-tolerance, which subsequently creates an environment that encourages the development of autoimmune diseases.
Pre-existing autoimmune disease
Researchers have discovered that a pre-existing Autoimmune disease can be a risk factor for developing future autoimmune diseases. While ongoing research is on to determine the relationship, scientists think the reason may be due to an alteration in the immune system by the initial disease.
Medications
Medications can increase the risks of the development of an autoimmune disease, e.g., drug-induced lupus. In this condition, drug exposure leads to the development of lupus in a genetically susceptible individual.
Infections
The presence of some infections may increase the risk of developing an autoimmune disease. For instance, studies have shown that there is a link between the Epstein Barr Virus infection and the development of Lupus. Another study also discovered the link between Group A Streptococcus and autoimmune diseases.
Cigarette and Other Toxins
Cigarette smoking has been associated with the development of multiple autoimmune disorders. These include Graves disease, SLE, multiple sclerosis, and rheumatoid arthritis. Apart from smoking, exposure to toxins from air pollutants, UV radiation, or organic solvents can also lead to the development of autoimmune diseases. Some toxic agents also have the ability to alter the genetic composition of a human, which can make them genetically more vulnerable to autoantibodies.
Common Autoimmune Disease Symptoms
Despite the diverse nature of autoimmune conditions, many of them present with similar signs and symptoms. You can find some of them in the table below:
| SYSTEM | SYMPTOMS |
|---|---|
| Digestive | • Abdominal cramps • Acid reflux • Diarrhea • Food intolerance • Nausea and Vomiting • Loss of appetite • Food sensitivities • Malabsorption • Constipation • Bloating |
| Cardiovascular | • Inflammation across joints • Heart failure • Arrhythmias • Myocardial injury • Hypertension • Coronary Artery Stenosis and Injury • Heart valve disease • Pericarditis |
| Musculoskeletal | • Inflammation across joints • Bone pain • Muscle weakness • Muscle Pain • Joint pain/stiffness/swelling • Osteomalacia |
| Nervous | • Anxiety • Impairment of Balance • Blurry vision • Depression • Memory loss • Migraines • Seizures • Numbness or tingling • Vision changes • Dizziness • Headaches • Brain fog • Compulsions, or phobias |
| Genitourinary | • Amenorrhea • Miscarriage • Infertility • Sexual dysfunction • Dysuria • Frequent urination • Bladder pain |
| Others | • Anemia • Fatigue • Fever • Mouth ulcers • Weight gain • Shortness of breath • Failure to thrive • Jaundice in newborn |
Symptoms of Autoimmune disease across different systems
The fact that there is no single test to diagnose most autoimmune disorders makes diagnosis challenging. Again, many of these symptoms are not exclusive to autoimmune disorders. Physicians have to combine observation findings with several other tests to make a diagnosis.

How is Autoimmune Disease Diagnosed?
From the extensive table of symptoms above, it is obvious that Autoimmune Disease can present in different forms. I remember my early days in medical school when one of our professors was teaching us about Systemic Lupus Erythematosus (SLE). He called it ‘the great masquerader’ because it can present like so many other illnesses.
This is the story of so many autoimmune diseases. They typically present with vague symptoms that would require a high index of suspicion on the part of a physician to diagnose.
That said, studies have been able to identify some specific tests and markers that may be present when autoimmune diseases are present. Therefore, a physician would typically request tests that may confirm or rule out the presence of an autoimmune disease. Some of these tests are:
Antinuclear Antibodies (ANA)
Antinuclear antibodies are types of autoantibodies that act on the nucleus of a cell. Different subtypes of ANA bind to diverse proteins within the nucleus.
Furthermore, they appear in autoimmune disorders, cancer, or infection. Hence, they can serve as markers of autoimmune diseases such as Systemic Lupus Erythematosus, Scleroderma, Sjorgren syndrome, Polymyositis, Autoimmune Hepatitis, Drug-induced Lupus, and Dermatomyositis. Testing for ANA will require a blood sample.
Autoantibody Tests
Autoantibodies can serve as markers of a disease process since the immune response is part of the disease. So when autoantibodies are in the circulation, it may be a pointer to the fact that an autoimmune disease process has started.
For instance, in Type 1 DM and thyroiditis, autoantibodies appear in the circulation years before the actual destruction of cells begins. Some diseases, such as diabetes, thyroiditis, and adrenalitis, may occur as autoimmune diseases or non-autoimmune. The presence of autoantibodies confirms autoimmune disease.
Immunofluorescence detects the presence of specific antibodies that confirm autoimmune diseases. But it gets a bit tricky because the same antibody may be present in several diseases. For instance, in the diagnosis of SLE, the Antinuclear antibody is typically present. But this same antibody is present in Rheumatoid arthritis, another autoimmune disorder.
C-reactive Protein (CRP)
The liver produces C-reactive protein in response to inflammation, usually during the acute phase of an inflammatory process. However, CRP levels rise in both acute and chronic conditions in response to infections, malignancies, tissue injury, and inflammatory and rheumatic conditions. Testing for this protein will require a blood sample.
Erythrocyte Sedimentation Rate (ESR)
The Erythrocyte Sedimentation Rate is a measure of how fast erythrocytes/Red Blood Cells (RBCs) settle at the bottom of a tube. For normal readings, RBCs take some time to settle, but when they are faster than normal, this indicates that there may be an inflammatory process going on. This test requires a blood sample.
Routine Tests
Other routine tests that can help to make a diagnosis include:
Comprehensive metabolic panel: can be useful in detecting autoimmune conditions like type 1 Diabetes and autoimmune hepatitis. This test measures the body’s metabolism, including electrolytes and minerals present in the blood. Expectedly, autoimmune diseases cause a derangement in the values of these electrolytes.
Complete Blood Count can detect anomalies in the white or red blood cells, which are seen in autoimmune diseases like SLE.
Coagulation studies can also be used to check the blood’s ability to clot, which can also be affected in autoimmune diseases like the antiphospholipid syndrome.
Biopsies and imaging may also be involved in making a diagnosis. Diagnosing Autoimmune disorders involves a combination of signs and symptoms and tests to rule out several other conditions that present similarly.
Now that you know about the symptoms and diagnosis of autoimmune diseases, let us discuss the role of diet.
What is the Autoimmune Disease Diet?
An Autoimmune disease diet, also known as the autoimmune protocol diet, helps to reduce the symptoms or prevent an autoimmune condition from getting worse than it is. While these diets may not cure the autoimmune condition, they can help individuals living with autoimmune diseases achieve a higher quality of life with low incidences or complete eradication of symptoms.
The Autoimmune Protocol (AIP) diet is a modified form of the paleo diet. This diet focuses on eliminating certain foods and Western dietary patterns that have been implicated in the dysfunction of the immune system and also Gastrointestinal disorders.
The Autoimmune disease diet works by limiting or avoiding foods that have been shown to trigger inflammatory reactions in the gut. It also works to prevent what is known as a leaky gut.
Leaky gut is a term used to describe an excess permeability of the gut lining. This means that normally, the gut lining is supposed to allow some amount of digested food substances and nutrients to get absorbed into the bloodstream.
However, when there is a disturbance in this structure, the gut can allow partially digested food, harmful microorganisms, and toxins to pass through. This is what is referred to as a ‘leaky gut.’ Moreover, this condition may trigger inflammatory and immune-mediated responses that occur within the gut and other parts of the body.
How Does the AIP Meal Plan Work?
The AIP Meal Plan Works via Three Stages:
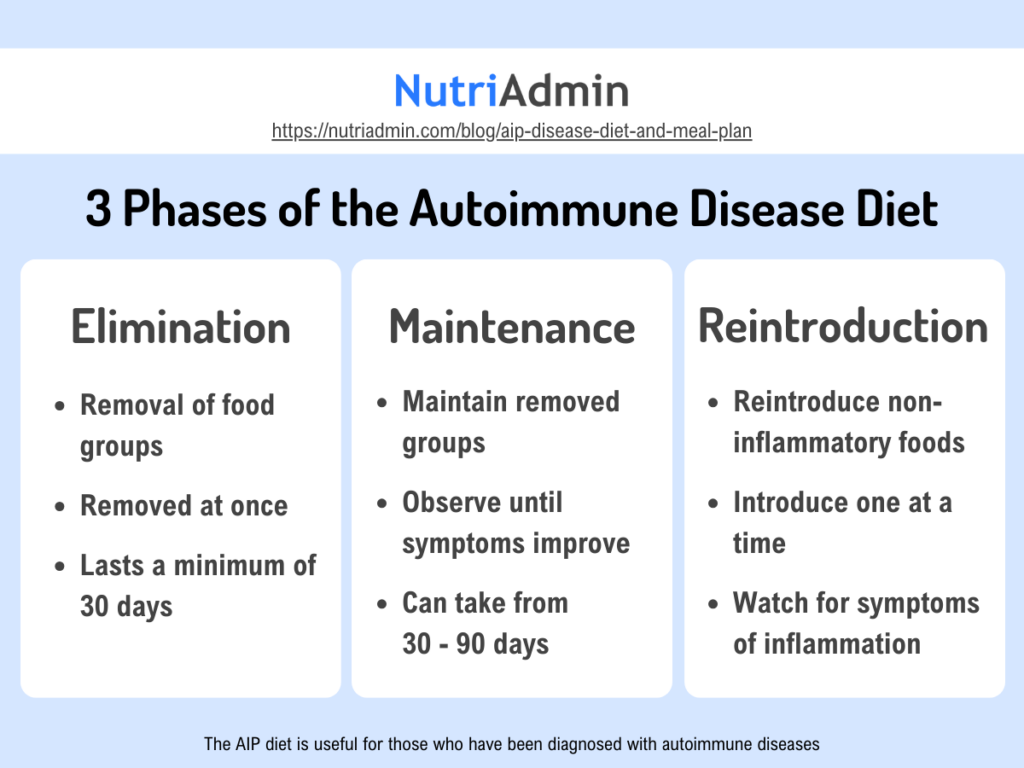
The Elimination Phase of the Autoimmune Disease Diet
This stage is to eliminate some foods that have been implicated in the development of a leaky gut. Some of these foods include gluten, refined sugar, grains, legumes, dairy, eggs, coffee, food additives, alcohol, nuts, seeds, and medications like NSAIDs.
It also addresses factors such as sleep, stress, and physical activity. Additionally, it focuses on preparing and consuming fresh, nutrient-dense foods, as well as fermented foods. This phase may be maintained for a minimum of 30 days.
The Maintenance Phase of the Autoimmune Disease Diet
This phase focuses on sustaining the changes in diet until the individual achieves a significant, measurable improvement in symptoms of the autoimmune condition. The duration of this phase may vary from 30 to 90 days. However, it does not matter how long it takes to see a significant improvement in symptoms. What matters is that the client avoids the eliminated foods throughout this phase.
The Reintroduction Phase of the Autoimmune Disease Diet
At this stage, there is a systematic, gradual introduction of food groups so that individuals with autoimmune conditions can identify foods that may worsen their symptoms. Foods that the individual tolerates well can be added to the diet, while those that trigger or worsen symptoms are still avoided.
In the reintroduction phase, note the following steps:
- Introduce one food group at a time every week.
- Begin with consuming one teaspoon of a particular food item, then observe your body’s reaction for about 15 minutes.
- If no adverse reactions are observed after 15 minutes, then increase the quantity you consume and wait for another 15 minutes.
- If there is still no adverse reaction after this, then eat a normal regular-sized portion of the food.
- Wait for the next 5 days to a week and observe your body’s response.
- Repeat the entire process with a new food item after a week.
It is advisable to work with a doctor while working with the autoimmune disease diet plan. A doctor can order some lab tests to help monitor some of the inflammatory markers as you work with your client to eliminate the wrong foods from their diet.
When to Recommend the Autoimmune Disease Diet
As a nutritionist or dietician, you can recommend the AIP diet plan to individuals with autoimmune diseases. It is specifically more suited for those who seem to have symptoms that are not well managed or keep getting worse over time.
Some diseases that may benefit from the Autoimmune disease diet include Fibromyalgia, Inflammatory Bowel Disease (Crohn’s Disease and Ulcerative Colitis), Celiac Disease, Hashimoto’s Thyroiditis, Grave’s disease, type 1 Diabetes, psoriasis, and other autoimmune diseases.

How to Make an AIP Meal Plan
Creating recipes and meal plans requires some level of expertise, and for autoimmune disease specifically, you must. Making AIP recipes and meal plans requires understanding foods to avoid and foods to include.
Foods Allowed in the Autoimmune Disease Diet
- Vegetables: Non-nightshade vegetables like leafy greens, broccoli, carrots, sweet potatoes, squash, beets, and others.
- Fruits: Most fruits, except for citrus fruits, which can be reintroduced later.
- Protein: High-quality meats, such as grass-fed beef, pastured poultry, wild-caught fish, and organ meats (in moderation).
- Healthy Fats: Avocado, coconut oil, olive oil, and animal fats from pastured sources.
- Bone Broth: Rich in nutrients and gut-healing properties.
- Fermented Foods: Sauerkraut, kimchi, kombucha (without added sugars), and other fermented foods to support gut health.
- Herbs and Spices: Except for seed-based spices (like cumin, coriander, and mustard), most herbs and spices are allowed.
- Non-Dairy Alternatives: Coconut milk and other non-dairy options like almond milk (without additives).
- Herbal teas with no caffeine. Common herbal teas like chamomile, peppermint, ginger, and rooibos are good options.
Foods to Avoid in the Autoimmune Disease Diet
- Grains: All grains, including wheat, rice, oats, and corn.
- Legumes: Beans, lentils, peanuts, and soy products.
- Nightshades: Tomatoes, potatoes, eggplants, and peppers (bell peppers, chili peppers, etc.).
- Dairy: All dairy products, including milk, cheese, and yogurt.
- Eggs: Eggs and egg-based products are excluded during the elimination phase but may be reintroduced later for some individuals.
- Nuts and Seeds: All nuts and seeds, including those used as flour or for cooking oil.
- Processed Foods: Processed foods, refined sugars, and artificial additives should be avoided.
- Alternative Sweeteners: Avoid sweeteners like stevia and artificial sweeteners during the elimination phase.
- Alcohol: Alcoholic beverages should be avoided due to their potential impact on gut health and inflammation.
- Coffee or caffeinated teas
AIP Meal Plan Generator
As a professional, you can create meal plans for your clients using several means, from paper and pen to Microsoft Word or a spreadsheet. However, to be more effective as a nutritionist or coach who creates specialized meal plans regularly, you may want to consider some software specialized for creating meal plans.
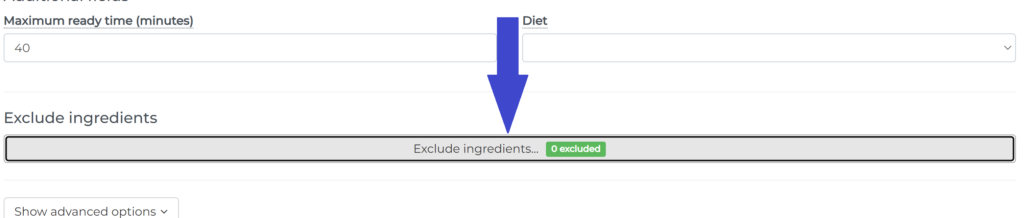
Moreover, several applications can help you create specialized meal plans in good time without reducing the quality of the plans. One of them is NutriAdmin. NutriAdmin provides a meal plan generator that allows you to create entire meal plans for a particular diet. In fact, this application supports 40+ diets, including the Autoimmune protocol diet.
The process is seamless, and you can have your autoimmune meal plan in just 60 seconds.
Here is a sample autoimmune disease meal plan generated by NutriAdmin.
Using the NutriAdmin meal plan generator, you can generate as many meal plans as you need. Every meal plan comes with AIP recipes which can be downloaded and also sent to your clients. The AIP recipes come with everything you need to prepare the meals, even down to the shopping list, so your client can prepare the meals step by step. NutriAdmin is easy to use, fast, and customizable, making it one of the best meal planning apps for professionals.
AIP recipes generated by NutriAdmin are not theoretical, impossible to cook meals. Rather they are super easy to cook in good time with a step-by-step guide fully explained. For the samples below, we used 40 minutes as the maximum cooking time. But it can go as low as 10 minutes if that is what you want.
a maximum of 40 minutes,
Here are some AIP recipes:
Benefits of the Autoimmune Disease Diet
Some research that was carried out among individuals with Inflammatory Bowel Diseases (IBD) showed that the AIP diet was able to improve their symptoms and reduce inflammation. Interestingly, this same benefit was also observed among individuals diagnosed with Hashimoto’s thyroiditis. This significant improvement in symptoms while using the AIP diet can happen as early as 3 weeks after its commencement.
Furthermore, the AIP meal plan also helps to discover food triggers that may worsen symptoms in inflammatory diseases so people with autoimmune disorders can avoid them.
It also helps you to create a customized meal plan that your clients can eat without fear of flares or triggers. You can use the NutriAdmin meal plan generator for this. This meal plan generator automatically excludes foods that are known to worsen autoimmune disease symptoms. However, it also has a section where you can manually exclude specific ingredients you don’t want in your client’s diet.
With the AIP meal plan, individuals diagnosed with autoimmune disorders can fully take control of their health and reverse some symptoms of the condition.
Does the Autoimmune Disease Diet have any Risks?
Yes, it does. However, the risk is very minimal if you work with your clients to use the autoimmune disease diet correctly. The greatest risk is developing nutrient deficiencies, which can occur during the elimination period where your client removes entire food groups from their diet.
Nutrient deficiencies usually occur when individuals get comfortable with a handful of select foods and eat only those for several weeks or months. However, with proper guidance from a doctor and nutritionist, you can prevent these nutrient deficiencies.
Another risk is that some people may rely too heavily on the diet to feel better and ignore other underlying causes. As explained earlier, autoimmune conditions have multifactorial causes. So, as much as possible, you should explore other causes of diseases along with your client. Working with a doctor and lab results would help you remove this risk and approach the condition holistically.
Self-care Tips for managing Autoimmune Diseases
Apart from diet, there are some things that your client can also do to alleviate symptoms of inflammation in autoimmune disease.
Exercise
Exercise can help to alleviate pain in the long term. However, a doctor’s supervision is essential, especially in people who have muscle or bone pain.
Stress Management
This is very crucial in the management of autoimmune disorders. Obviously, stress and anxiety can trigger flares in autoimmune conditions. Therefore, encourage your client to avoid stress as much as possible. Relaxation techniques, work pacing, and meditation are good ways to deal with stress. Getting enough rest is also key in managing stress symptoms.
Support groups
A well-coordinated community that is big on positivity can boost mental health and help recovery in autoimmune disorders. Moreover, managing autoimmune conditions can be very stressful especially when people around do not understand what is going on. Therefore, it is important to get people that understand what the condition is and connect with them.

Sleep
A lot of cell repair goes on during sleep. Sleep deprivation prevents or limits this process and can even be a trigger for autoimmune flares. Therefore, sleeping well is not negotiable.
Hydration
Staying hydrated is key when it comes to the management of autoimmune conditions. Take enough water to prevent dehydration which can be a trigger for flares. Taking enough water can also help to relieve symptoms.
Medications
Take your medications when due. The AIP meal plan is not against the use of medications. The goal of both medications and a healthy diet is to make you well and relieve symptoms. So, cooperate with your doctor to achieve optimal health.
Conclusion
A diagnosis of an autoimmune disorder is not a life sentence to pain and discomfort. Research has shown over and over that the autoimmune disease diet is effective at combatting some of the symptoms of this condition.
With the right approach to diet, nutrition, and supervision by healthcare professionals, people with autoimmune diseases can still maintain a high quality of life.
Additionally, it is important to also state that the AIP diet is not against medical interventions of any kind. It can work synergistically with medical science to boost the quality of life and reduce symptoms of autoimmune conditions.