In recent years, there has been a growing interest in gut microbiome and its connection with our diet. This surge in interest is due to the increasing recognition of the connection between the gut microbiota and human health. Many nutrition and health professionals have started specializing in this field, and you might wonder why.
The reason is clear: gut microbiota play a crucial role in various health outcomes. They influence the immune system, heart and metabolic health, digestion, and mental well-being. This increased awareness emphasizes the need to understand and nurture our gut health for overall well-being.
The Gut Microbiome
The human microbiome encompasses trillions of microorganisms, including bacteria, fungi, parasites, and viruses. It is the collection of microbes, their genes, and their products that colonizes our body from birth and transfers from one generation to the next.
In a healthy individual, these diverse species peacefully coexist, primarily residing in the small and large intestines but also distributed throughout the body, forming the intricate web known as the microbiome.
How does the microbiome develop in our body?
The development of the microbiome in our body starts with the initial exposure to diverse microorganisms at birth and further evolves through interactions with external factors such as food and the environment.
In the womb, our mother’s body and immune system actively shield us from various foreign microorganisms, ensuring a sterile environment. Upon the rupture of the amniotic sac and our entry into the world, we come into contact with bacteria.
During a vaginal delivery, we acquire microbes from the birth canal, whereas a cesarean section exposes us to our first dose from the skin of our caregivers.
Upon birth, we quickly encounter diverse bacteria from various sources. These microbes, surpassing our own cells within days, create differences in babies’ microbial communities.
During the first six months, infants exhibit significant microbial diversity.
As infants grow, diverse foods and their curious habit of touching and putting things in their mouths introduce new gut microbes.
Between six months and three years, a stable microbiome forms, aligning with an adult-like diet and immune development completion. By adulthood, gut microbes become more similar, remaining stable for over a year but with species abundance variations.
Throughout life, factors such as disease, age, diet, location, and the intake of supplements or drugs, including antibiotics, influence our gut microbiome. These factors contribute to unique gut microbiota in individuals and distinct differences between populations.
Microbes from Mouth to Gut
Have you ever wondered about the journey of microbes from our food? What exactly happens to them along the way?

Millions of microbes, present in the oral and saliva microbiomes, accompany our daily food intake. However, their survival in the gut encounters challenges from stomach acidity, bile acids, and digestive enzymes.
In the small intestine, a gradient of microbes is evident. Predominantly oxygen-tolerant types characterize the upper part, transitioning to mostly anaerobic bacteria in the lower gut.
The colon, succeeding the small intestine, is dominated by anaerobic bacteria, impacting overall health and associated with various diseases. Living without a colon is possible, but the small intestine, crucial for digestion and nutrient absorption, is indispensable.
The duodenum, a segment of the small intestine, and its microbes have become prominent factors in metabolic and potentially immune diseases.
Significance of a Healthy Gut Microbiome
A healthy gut flora significantly contributes to the overall health of a person. It performs crucial functions such as aiding in nutrient metabolism, processing drugs and foreign substances, maintaining the integrity of the gut mucosal barrier, modulating the immune system, and protecting against harmful pathogens.
Immune Function
The gut is crucial for immune regulation because about 70% of the entire immune system is located there. Additionally, about 80% of plasma cells, crucial for producing IgA antibodies in immune defense, are situated in the gut’s lamina propria.
The gut microbiome plays a crucial role in shaping and maintaining the immune system. This symbiotic relationship is essential for a well-functioning immune system that effectively responds to threats and maintains tolerance to harmless substances.
Mental Health
A healthy gut is linked to normal central nervous system (CNS) function, with signals sent to the brain through the gut-brain axis (GBA).
The brain directly impacts the stomach and intestines. Just the thought of eating or catching a whiff of something delicious, like freshly baked bread, can prompt stomach juices even before the food is present, highlighting the brain’s influence.
This connection works both ways — a distressed intestine can signal the brain, just as a troubled brain can affect the gut. This means stomach issues can be both the cause and result of anxiety, stress, or depression, highlighting the close link between the brain and the gastrointestinal system.
Gut microbiota actively influences mental health by playing a crucial role in neurotransmitter production essential for brain function. For instance, the microbiome actively produces 90% of serotonin, a neurotransmitter linked to depression and other mental health disorders.
Anxiety disorders, characterized by excessive worry and physical symptoms, show reduced bacterial diversity in the gut microbiome. Some studies also show that treatments correcting the gut microbiome composition, like diet and probiotics, show effective management of anxiety symptoms.
Weight Management
The gut microbiome plays a crucial role in weight management. Specific bacteria in the gut can break down carbohydrates, producing fatty acids that the body uses for energy. Individuals with more of these bacteria may extract more energy from food, leading to weight gain.
Additionally, gut bacteria influence appetite by producing hormones that affect feelings of hunger and fullness. For example, some bacteria stimulate the release of appetite-suppressing hormones.
Moreover, the gut microbiome influences metabolism, and the communication between the gut and the central nervous system can impact eating behavior and metabolism, affecting weight management.
Nutrient Metabolism
Carbohydrates
The gut microbiota digest fiber, fermenting them into short-chain fatty acids (SCFA) like butyrate, propionate, and acetate. These SCFAs interact with receptors and hormones, affecting our energy balance. Butyrate also helps prevent the build-up of harmful by-products.
Microbes like Bacteroides, especially Bacteroides thetaiotaomicron, use enzymes to process carbohydrates, and they have more enzymes than our human genome. The gut microbiota also helps counter the formation of kidney stones by dealing with oxalate produced during carbohydrate fermentation.
Proteins
The gut microbiota has a powerful system for processing proteins, involving microbial proteinases, peptidases, and human proteinases.
Amino acid transporters on bacterial cell walls allow amino acids from the gut to enter bacteria, where gene products convert them into signaling molecules and antimicrobial peptides (bacteriocins).
Lipids
The gut microbiota positively influences lipid metabolism by enhancing lipoprotein lipase activity in fat cells. Specifically, Bacteroides thetaiotaomicron boosts the effectiveness of lipid breakdown by increasing the expression of a colipase, crucial for pancreatic lipase in digesting fats.
Other Nutrients and Compounds
The gut microbiota plays a crucial role in synthesizing vitamin K and various components of vitamin B. Bacteroides, a bacterial genus, is known to produce conjugated linoleic acid (CLA), recognized for its health benefits such as anti-diabetic, anti-atherogenic, anti-obesogenic, hypolipidemic, and immunomodulatory properties.
Additionally, research indicates that the human gut microbiota is crucial in breaking down polyphenols found in plants, fruits, and products like tea and cocoa.
These compounds, including flavonoids, are initially bound to sugars and transformed into active forms by the gut microbiota. After this process, the active products are absorbed and travel to different tissues, exhibiting antimicrobial and metabolic effects.
Gut Microbiome Dysbiosis
Numerous factors can actively influence our gut microbiome, both positively and negatively. Dysbiosis, characterized by changes in gut microbiota composition and function, including a decrease in diversity and the presence of harmful microbes, results from various factors.

Factors like genetics, health, and lifestyle, as well as environmental influences such as diet, drugs, and hygiene, can contribute to dysbiosis. Specifically, high sugar and low fiber diets, along with the use of antibiotics and certain drugs, are known contributors.
While some are beyond our control, others—such as diet, lifestyle, and stress—are within our ability to manage.
Antibiotics
Antibiotics, while vital, have unintended consequences on the gut microbiome. A study on healthy volunteers showed that even short antibiotic courses lead to a significant and lasting alteration of the gut microbiota. Some individuals showed persistent alterations resembling the gut microbiomes of intensive care unit (ICU) patients.
Additionally, antibiotic use increases the prevalence of antibiotic resistance genes in the gut, posing potential risks. It is important to consult your doctor first before taking any antibiotic medicines.
Food Additives
Recent research has highlighted the impact of food additives on the gut microbiota. Preservatives, in particular, have been found to sensitively affect some human gut bacteria, leading to the overgrowth of proteobacteria.
Additionally, categories like emulsifiers and artificial sweeteners have been shown to have negative effects on human health. Emulsifiers directly modify the composition of the gut microbiota and trigger intestinal inflammation, while artificial sweeteners contribute to proteobacterial dysbiosis and worsen ileitis in a study involving mice.
Despite being introduced to prevent metabolic syndrome, non-caloric artificial sweeteners paradoxically induce dysbiosis and promote glucose intolerance in a microbiota-dependent manner, resulting in the opposite of their intended metabolic benefits.
Lifestyle
Lifestyle factors strongly influence gut health. Regular exercise has a positive impact, promoting a diverse and balanced gut microbiome. Quality sleep supports gut health by allowing the body to repair and regenerate. Effective stress management is crucial, as chronic stress can disrupt the balance of gut bacteria.
Tobacco use has adverse effects, contributing to inflammation and negatively affecting the gut. Excessive alcohol consumption can disrupt the gut microbiota, leading to inflammation and impaired digestion. Adopting a healthy lifestyle, including regular exercise, sufficient sleep, stress reduction, and limiting tobacco and alcohol intake, plays a vital role in maintaining optimal gut health.
Stress
Psychological stress and depression can lead to the consumption of highly palatable foods, influencing the types of gut bacteria that flourish. Moreover, stress and depression can alter the composition of gut bacteria through factors like stress hormones, inflammation, and autonomic changes.
These bacteria, in turn, release substances that can impact eating behavior and mood, including metabolites, toxins, and neurohormones. Some bacterial species may contribute to dysregulated eating patterns.
Additionally, gut bacteria may increase stress responsiveness and the risk of depression, a risk that probiotic supplementation could potentially reduce. The following are some tips to help you manage stress:
- Deep Breathing: Inhale slowly, hold, and exhale to calm your nerves.
- Exercise Regularly: Physical activity releases mood-lifting endorphins.
- Mindfulness Meditation: Focus on the present moment to reduce anxiety.
- Establish a Routine: Create a daily plan for structure.
- Adequate Sleep: Ensure quality sleep for stress reduction.
- Healthy Diet: Eat a balanced, nutritious diet for an improved mood.
- Social Connections: Stay connected with friends and family for emotional support.
- Time Management: Prioritize tasks to avoid feeling overwhelmed.
- Hobbies and Relaxation: Engage in enjoyable activities for relaxation.
- Learn to Say No: Set limits to avoid overcommitting.
- Positive Self-Talk: Challenge negative thoughts with positive affirmations.
- Limit Stimulants: Reduce caffeine and nicotine intake, especially before bedtime.
- Seek Professional Help: Consult a mental health professional if stress becomes overwhelming.
Smoking
Smoking, particularly through the consumption of nicotine in tobacco, can influence gut health by altering the gut microbiome. In both animal and human studies, nicotine has been associated with changes in the composition of gut bacteria, specifically, reduced microbial diversity, compared to non-smokers. Notably, smoking cessation can induce significant shifts in the gut microbiome, indicating its responsiveness to changes in tobacco exposure.
Alcohol
Alcohol consumption, particularly in the form of ethanol in alcoholic beverages, is shown to alter the gut environment and modulate the composition of gut microbiota, contributing to the development of alcohol-related diseases.
In a recent study related to binge drinking and gut microbiome in young adults, it showed the link between binge drinking episodes and alterations in gut bacteria, influencing the immune response and substances involved in gut-brain communication. More binge drinking is connected to higher impulsivity and difficulties in emotional recognition and processing speed.
The study also finds a connection between cravings and specific gut bacteria changes, indicating potential early markers for addictive behavior. Overall, these findings highlight how alcohol can affect the gut microbiome in young binge drinkers, possibly increasing the risk of mental health issues during the crucial developmental phase of adolescence.
Exercise
Exercise actively influences gut health by impacting the composition of the gut microbiome. Physical inactivity is associated with a less diverse and imbalanced gut microbiota, potentially leading to a reduction in beneficial bacteria.
This imbalance may contribute to digestive issues, compromised immune function, and increased susceptibility to inflammation in the gut. Additionally, sedentary behavior is linked to conditions such as constipation and a higher risk of gastrointestinal disorders.
Low-intensity exercise, for example, reduces transient stool time, providing protective effects against conditions like colon cancer and inflammatory bowel disease. Voluntary exercise is associated with variations in microbiota composition and an increase in beneficial substances like n-butyrate, positively affecting cognitive abilities. Regular controlled exercise contributes to the improvement of the gut microbiota composition, potentially serving as a therapeutic approach for conditions like obesity and hypertension.
In humans, exercise actively enhances microbial diversity, particularly among beneficial taxa, highlighting its active role in maintaining a healthier intestinal environment. Overall, exercise actively plays a positive role in modulating the gut microbiome, actively contributing to better gut health and potentially influencing various aspects of overall well-being.
Sleep
Sleep, a crucial part of our daily routine, accounts for almost one-third of our time and plays a pivotal role in essential bodily functions such as cognitive performance, memory consolidation, and mood regulation.
Unfortunately, many people experience sleep deprivation due to factors like poor diet, stress, and excessive smartphone use. This lack of sleep has been linked to various health issues, including depression, obesity, diabetes, cardiovascular diseases, and even an increased risk of death.
Lack of sleep is known to contribute to immune and metabolic diseases, and recent evidence highlights the link between disrupted sleep and imbalances in gut microbiota, which play a role in these conditions.
When it comes to sleep, studies reveal that sleep deprivation can disturb the balance of gut microbiota, resulting in dysbiosis. This imbalance is characterized by a reduction in beneficial bacteria and an increase in potentially harmful ones.
The importance of adequate sleep for maintaining a healthy gut microbiota and overall well-being cannot be overstated. Getting enough sleep ensures that the diverse community of microorganisms in our gut remains in harmony, positively impacting various bodily systems. In essence, prioritizing quality sleep is a fundamental step towards supporting both physical and mental health.
Tips to Help Improve Sleep
- Maintaining a consistent sleep schedule by going to bed and waking up at the same time each day can regulate the body’s internal clock, enhancing overall sleep quality.
- Creating a relaxing bedtime routine, incorporating activities such as reading or gentle stretching, signals the body that it’s time to wind down.
- Ensuring a comfortable sleep environment, with a cool, dark, and quiet bedroom along with a supportive mattress and pillows, contributes to uninterrupted sleep.
- Limiting screen time before bedtime, due to the blue light emitted by devices, helps in promoting the natural sleep-wake cycle.
- Engaging in regular physical activity, preferably earlier in the day, has been linked to better sleep.
- Managing stress through practices like meditation or deep breathing positively influences sleep patterns.
- Avoid consuming food or drinks with caffeine like coffee or chocolates before bedtime.
The Impact of Diet on the Gut Microbiome
The food we eat not only provides nutrients to our body but also fuels the gut microbiome in our gastrointestinal tract.

One of the most influential factors shaping the functions and composition of the gut microbiota is diet. The intricate relationship between diet, the immune system, and the intestinal barrier emphasizes the central role of nutrition in both the development and treatment of numerous diseases.
Eating a variety of foods, especially different plants, is good for the microbes in your gut. Studies have found that a diverse diet supports the growth of various helpful microbes.
Dietary Fiber
In recent years, research has increasingly highlighted the positive effects of consuming dietary fiber on overall well-being. However, there has been a significant decline in dietary fiber intake over the centuries, contributing to harmful changes in the gut microbiota.
As people have reduced their consumption of dietary fiber, the gut microbiota has undergone detrimental alterations. This shift is linked to the rising global prevalence of noncommunicable diseases such as diabetes and cancer.
The gut microbiome drives the fermentation of fiber in the colon, and, in turn, the nutritional substrate of intestinal flora can influence the structure and diversity of the microbiome. Certain dietary fiber sources are fermentable, providing growth substrates for microbes in the distal bowel. Some non-digestible carbohydrates are called “prebiotics”, defined as components that are not digestible by the human body but selectively nourish beneficial colonic microorganisms.
The gut microbiota responds differently to varying types, quantities, and durations of dietary fiber intake. Each person exhibits unique tolerances to specific types and amounts of dietary fiber, emphasizing the necessity for personalized dietary interventions.
Fats
A high-fat diet, especially saturated fats, reduces microbial diversity, and may promote an inflammatory state. In a systematic review in 2019, it showed that diets high in saturated fats can have negative effects on gut health and metabolism. Similarly, diets rich in monounsaturated fats may also impact the gut negatively, while polyunsaturated fats appear not to have such adverse effects.
It’s important to note that existing data are inconsistent, with many studies showing potential biases.
Proteins
The majority of dietary protein sources can be broadly categorized into two groups: plant-derived protein and animal-derived protein. Plant-based protein is generally considered to have lower digestibility compared to animal-based protein.
A recent review, which conducted a literature search of clinical trials published until February 2023, explored the impact of various macronutrients and dietary patterns on the gut microbiota in individuals with overweight and obesity. The findings suggest that increased consumption of animal protein and adherence to a Western diet may contribute to a decline in beneficial gut bacteria and an elevation in harmful ones commonly associated with obesity.
Conversely, diets abundant in plant proteins, exemplified by the Mediterranean diet, demonstrate a notable rise in anti-inflammatory bacteria producing butyrate, enhanced bacterial diversity, and a reduction in pro-inflammatory bacteria.
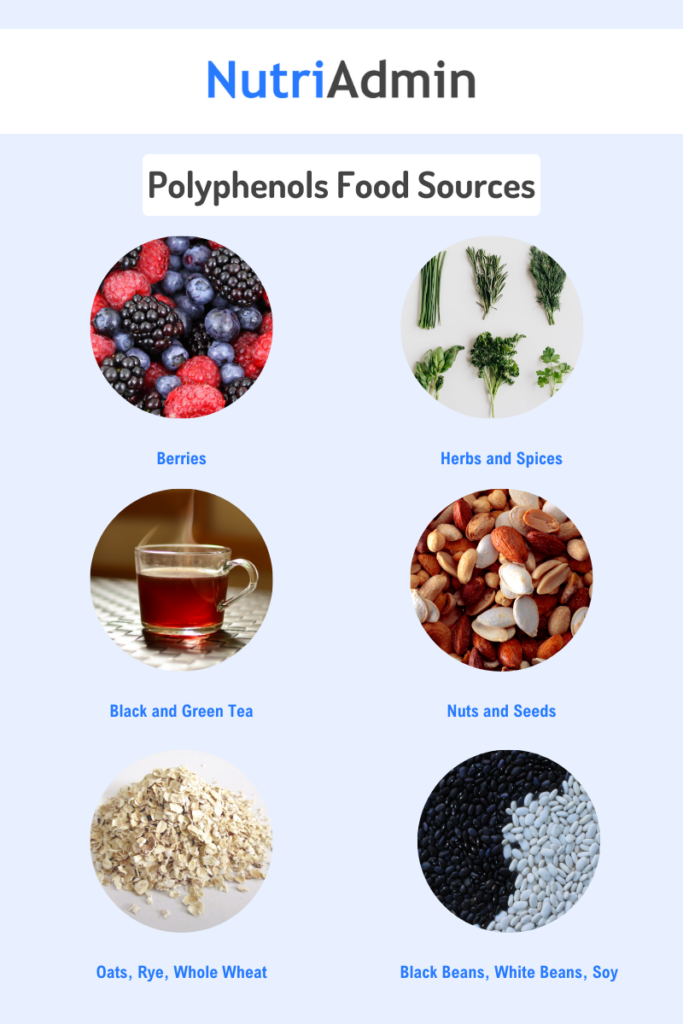
Polyphenols
Polyphenols are natural compounds found in plants with diverse benefits. There are more than 8,000 types of polyphenols in plants. They can reduce free radicals, oxidative stress, DNA damage, and inflammation, potentially slowing down aging and preventing age-related diseases.
When we eat foods containing polyphenols, our bodies don’t absorb them very well compared to micro- and macronutrients. Most of the polyphenols (about 90-95%) don’t get absorbed in the small intestine, so they end up in the large intestine, where they interact with gut microbes.
This interaction acts as prebiotics, fostering beneficial bacteria growth, and exhibits antimicrobial properties against harmful gut bacteria.
Common Polyphenols
Flavonoids
Flavonoids, a class of polyphenol phytochemicals, play a crucial role in inhibiting inflammation in various animal models of chronic disease. They combat intestinal inflammation, linked to chronic diseases such as cardiovascular disease, diabetes, Alzheimer’s disease, inflammatory bowel disease, and colon cancer, as highlighted by numerous studies.
Stilbenes
This type of polyphenol is not common in our diet but are found in plants as antifungal phytoalexins, produced in response to infection or injury. Resveratrol, a well-known stilbene, is naturally present in grapes, and it’s also found in red wine.
A 2022 review underscores resveratrol’s significance in safeguarding intestinal barriers, showcasing its capacity to withstand damage and uphold functionality. With antioxidant, anti-inflammatory, anti-cancer, and cardiovascular protective properties, resveratrol affects absorption and metabolism in the gastrointestinal tract. Moreover, resveratrol exhibits promise in addressing and preventing diverse intestinal-related conditions, such as Inflammatory Bowel Disease (IBD), Colorectal Cancer (CRC), Irritable Bowel Syndrome (IBS), and infectious diseases.
Lignans
Lignans, when converted by the gut microbiota into active compounds, particularly enterolignans like enterolactone and enterodiol, play crucial roles in important bodily processes. These compounds contribute significantly to reducing inflammation, countering oxidative stress, activating estrogen receptors, and influencing gene expression or enzyme activity.
Recent evidence indicates that lignan-rich diets provide protection against health issues like colorectal and breast cancer, as well as cardiovascular diseases. However, variations in gut microbiota’s activation of lignans can occur due to factors such as diet, food transit time, and intestinal redox state.This leads to notable differences in enterolignan concentrations in urine, feces, and blood among individuals.
Lignans are present in various plant families, with varying types and amounts. They are abundant in whole grains, particularly in the bran layer, and seeds, including barley, buckwheat, oats, rye, sesame seeds, and wheat. Nuts and legumes also serve as good sources. Additionally, fruits and vegetables, including asparagus, grapes, kiwi, lemons, oranges, as well as coffee and tea, contain lignans, albeit in smaller quantities than grains.
Tips for Improving Gut Health through Diet
Maintaining a healthy gut microbiome is crucial, and one effective approach is to give importance to a balanced diet. A balanced and nutritious diet helps maintain a healthy community of microorganisms in your gut, supporting good digestion and overall well-being.

Incorporate a Variety of Foods Into Your Diet
Our gut comprises various types of microbes, each with its preferred food sources. To explain it simply, some microbes may thrive on green leafy vegetables, while others may prefer beans or fruits. To support the flourishing of these diverse microbes in our gut, it’s essential to incorporate a variety of foods into our diet.
In practice, the best way to promote a healthy microbiome is to include a broad spectrum of fresh, wholefoods in our diet, with a focus on plant sources such as fruits, vegetables, legumes, beans, nuts, and whole grains. This approach ensures that we provide the necessary nutrients to support the different microbes in our gut, contributing to overall gut health.
Increase Fiber Intake
As mentioned earlier, dietary fiber is beneficial to our gut microbiome and overall health. The Academy of Nutrition and Dietetics advises that individuals should aim for 14 grams of dietary fiber for every 1,000 calories consumed daily.
Specifically, women should target around 25 grams, while men should aim for approximately 38 grams of dietary fiber each day. It’s important to note that individual requirements may differ based on energy needs.
Tips to Increase Fiber Intake
- Choose Whole Grains: Opt for whole grain bread, brown rice, quinoa, and whole wheat pasta instead of their refined counterparts.
- Include Legumes: Beans, lentils, and peas are excellent sources of fiber. Add them to soups, salads, or main dishes.
- Eat More Vegetables: Incorporate a variety of vegetables into your meals. Include dark, leafy greens, broccoli, carrots, and bell peppers.
- Snack on Fruits or Vegetables: Have fresh fruits, such as apples, berries, or pears, as snacks. Leave the skin on for added fiber. Snacking on vegetables like celery sticks is also a great way to add fiber to your diet.
- Eat Fruits Whole: Eating fruits whole, rather than juicing them, ensures you get the full benefit of their fiber content. Blending fruits into smoothies retains some fiber, but maximizing the nutritional value of fruits occurs when you enjoy them in their natural state.
- Nuts and Seeds: Snack on a handful of almonds, chia seeds, or flaxseeds. They’re not only nutritious but also high in fiber.
- Choose High-Fiber Cereals: Look for cereals with high fiber content. Check the nutrition labels when buying.
- Use Whole Ingredients: When cooking or baking, use whole ingredients. For example, choose whole wheat flour instead of refined white flour.
Remember to gradually increase fiber intake to give your digestive system time to adjust. It is also important to stay hydrated when increasing fiber in your diet to prevent constipation, facilitate digestion, reduce discomfort, and support a balanced gut microbiome.
If you have any health concerns, it’s always a good idea to consult with a healthcare professional or a registered dietitian to give you individualized advice.
Consume 30 Types of Plants a Week
In 2018, the American Gut Project conducted a study revealing that individuals who consume 30 or more types of plants in their diet per week tend to have greater diversity in their gut microbiome compared to those who consume fewer than 10 types of plants.
Consuming 30 types of plants per week not only introduces a variety of foods into your diet but also helps in increasing your fiber intake. This approach effectively incorporates the previously mentioned tips for maintaining a healthy gut.
Eating 30 types of plants might sound challenging, but it’s not just about fruits and vegetables. This includes various plant-based foods like grains, nuts, seeds, beans, and legumes.
Dr. Megan Rossi, also known as The Gut Health Doctor, has introduced an innovative approach called the 30 Plant Point system, designed to be accomplished within a week.
This system simplifies the goal of consuming 30 types of plants weekly by assigning plant points to different types of plants. By following this structured system, individuals can effectively track their progress and ensure they achieve the target of 30 plants a week for optimal gut health. According to the The Gut Health Doctor website, each plant counts as 1 point, while olive oil, tea, coffee, herbs and spices count as ¼.
To help you track the number of plants you consumed for the week, you can download the checklist below:
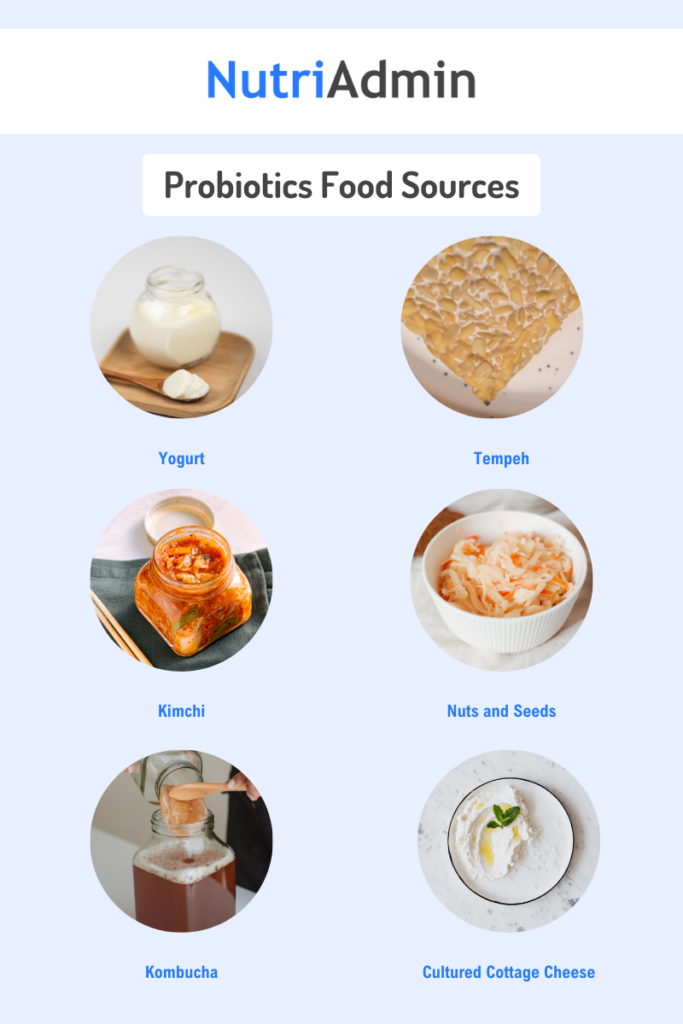
Consume Fermented Foods
Fermented foods undergo a preservation method that not only extends shelf life and enhances nutritional content but also introduces beneficial probiotics—living microorganisms—to support your health.
Foods rich in beneficial probiotics include those naturally fermented, such as yogurt, kefir, kimchi, sauerkraut, and some pickles. However, it is important to note that not every fermented or pickled food contains probiotics. For instance, some store-bought pickles, pickled with vinegar instead of natural fermentation, may lack probiotics. Ensure to choose foods labeled as “naturally fermented.”
A research review in 2022, states that fermented foods can influence the gut microbiome, impacting it both in the short and long term.The following are some fermented food items that were mentioned on the review and its effect on our health:
- Fermented dairy products – connection with effective weight management, reduce risks of cardiovascular disease and diabetes, and positive effects on glucose metabolism from fermented milk after exercise.
- Kimchi – linked to anti-diabetic and anti-obesity effects
- Sauerkraut – intake in IBS patients demonstrated notable improvements in symptoms and a significant alteration in the gut microbiota composition.
Including fermented foods in your diet can benefit the gut microbiome by supplying nutrients and introducing beneficial microbes. However, researchers need to conduct more studies to precisely uncover the influence of fermented foods on the gut microbiome.
Prebiotics and Probiotics
When discussing gut health, we often mention prebiotics and probiotics because they greatly impact our gut microbiome. So, what’s the difference? How do they affect our microbiome?
Prebiotics are substances that promote the growth and activity of beneficial bacteria in the gut. They serve as a food source for these bacteria, aiding in their proliferation and maintaining a healthy balance in the microbiome.
Probiotics, on the other hand, are live beneficial bacteria that, when consumed, confer health benefits to the host. They contribute to the overall diversity and equilibrium of the gut microbiota, promoting digestive health and supporting the immune system.
Both prebiotics and probiotics play crucial roles in fostering a balanced and thriving gut environment, essential for overall well-being. Consuming a diet rich in prebiotic and probiotic-containing foods can contribute to optimal gut health.
| Prebiotics | Probiotics |
|---|---|
| • Non-digestible fibers that serve as food for our gut bacteria, promoting their growth and activity. It enables probiotics to grow and function. Without prebiotics, probiotics cannot thrive or multiply. | • Foods or supplements containing live microorganisms that offer health benefits when consumed in sufficient amounts. |
| Food sources: vegetables, fruits, whole grains, legumes, nuts and seeds | Food sources: some fermented foods like yogurt, kefir, uncooked sauerkraut, traditional kimchi, tempeh, miso, kombucha, natto, pickles |
Conclusion
The gut microbiome, a community of trillions of microorganisms, significantly impacts our health. It begins developing at birth, influenced by factors such as delivery mode and early exposure to microbes.
A healthy gut microbiome plays a crucial role in various functions, from immune regulation to mental well-being. Nutrition strongly influences it—eating a balanced, diverse diet with fiber-rich and plant-based foods supports beneficial bacteria.
Conversely, factors like a high-fat diet, antibiotics, and a sedentary lifestyle can lead to gut dysbiosis. Sleep, an essential part of daily life, is also crucial for maintaining a healthy gut microbiota.
Practical steps to support gut health include incorporating a variety of foods, increasing fiber intake, consuming 30 types of plants weekly, and adding fermented foods. Recognizing the roles of prebiotics and probiotics, addressing lifestyle factors like stress, exercise, and avoiding smoking contribute to optimal gut health.
In essence, prioritizing gut health through lifestyle choices and a nutritious diet is key to overall well-being.
Example Meal Plan for Gut Health
NutriaAdmin is an all-in-one software designed specifically for nutrition and fitness professionals. One of the software’s major feature, the meal plan generator, is made to help create customized meal plans in just 60 seconds.
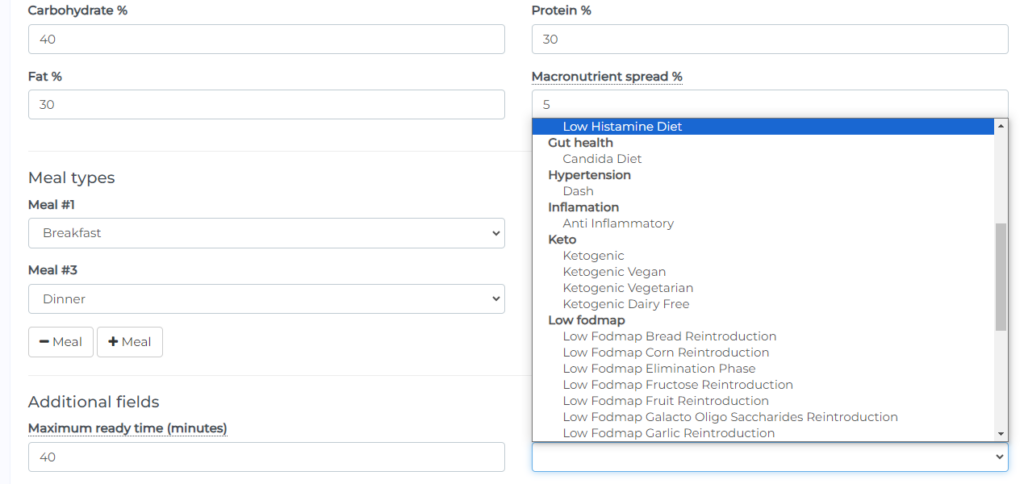
The meal plan generator includes filters that allow you to choose calories, macros, maximum ready time, ingredients you want to exclude, cooking equipment, cuisines, and specific diets, such as the Mediterranean diet known for promoting gut health. Additionally, there are diets like the Candida Diet and Low Fodmap Diets, tailored to alleviate symptoms for individuals with gut issues, along with 40 other diet options, enabling a versatile and customized approach to meal planning and recipe generation.
Here’s a 7-Day sample Candida Diet meal plan from NutriAdmin’s Meal Plan Generator: